Sleep apnea is a common sleep disorder that affects millions of people worldwide, but have you ever wondered what actually causes it? In this article, we will unravel the mystery behind this condition and explore the various factors that contribute to its emergence. From lifestyle choices to genetic predisposition, we will shed light on the underlying causes of sleep apnea and delve into the potential solutions for a better night’s sleep. So, if you’ve ever found yourself struggling to breathe during sleep or know someone who does, read on to discover the secrets behind this often-unseen enemy. Sleep apnea is a common sleep disorder that affects millions of people around the world. It is characterized by interrupted breathing during sleep, causing a person to briefly wake up multiple times throughout the night. This can lead to daytime sleepiness, fatigue, and other health issues. Understanding the causes of sleep apnea is crucial in developing effective treatment plans.
Review contents
Obstructive Sleep Apnea (OSA)
Excess Weight
One of the leading causes of obstructive sleep apnea is excess weight. When we carry extra weight, it can lead to the accumulation of fatty tissues around the neck and throat area. These tissues can block the airway during sleep, causing apnea episodes. Losing weight through a combination of healthy eating and regular exercise can significantly reduce the severity of sleep apnea or even eliminate it altogether.
Obesity
In connection to excess weight, obesity itself is a risk factor for sleep apnea. Obesity is defined as having a body mass index (BMI) of 30 or higher. The excess fat can restrict the upper airway and cause breathing difficulties during sleep. Managing obesity through lifestyle changes, such as adopting a balanced diet and engaging in physical activity, can positively impact sleep apnea symptoms.
Upper Airway Obstructions
The upper airway can become narrowed or obstructed due to various factors. Structural abnormalities, such as a deviated septum or enlarged adenoids, can impede airflow, leading to sleep apnea. Additionally, certain lifestyle choices such as smoking or nasal congestion can contribute to upper airway obstructions. Identifying and addressing these underlying issues can aid in the management of sleep apnea.
Enlarged Tonsils or Adenoids
Enlarged tonsils or adenoids are commonly associated with sleep apnea, especially in children. These glands can obstruct the airway, causing recurring apnea episodes during sleep. In such cases, surgical removal of the tonsils or adenoids may be necessary to alleviate the symptoms of sleep apnea.
Nasal Congestion
Nasal congestion, whether due to allergies, sinus infections, or anatomical factors, can contribute to sleep apnea. When the nasal passages are blocked, it forces individuals to rely more on breathing through their mouth, increasing the likelihood of airway collapse during sleep. Addressing nasal congestion through medications or treatments like nasal sprays or allergen avoidance can help improve sleep apnea symptoms.
Smoking
Smoking has detrimental effects on overall health, and it can also contribute to sleep apnea. The chemicals in tobacco smoke can cause inflammation and irritation in the upper airway, leading to increased airway resistance and obstruction. Quitting smoking can significantly improve sleep apnea symptoms and promote better overall respiratory health.
Alcohol and Sedative Use
Alcohol and sedatives are known to relax the muscles in the body, including those in the throat and tongue. This relaxation can increase the likelihood of airway collapse and obstruction during sleep, leading to sleep apnea episodes. Limiting alcohol consumption, especially close to bedtime, and avoiding sedatives can help minimize the impact of these substances on sleep apnea.
Central Sleep Apnea (CSA)
Brainstem Problems
Central sleep apnea is primarily caused by problems in the brainstem, which controls the breathing process during sleep. If the brainstem fails to send the proper signals to the muscles involved in respiration, it can cause interruptions in breathing. Brainstem problems can be attributed to various factors such as brainstem injury, stroke, or certain medical conditions.
Congestive Heart Failure
Congestive heart failure is a condition in which the heart is unable to pump blood efficiently, leading to fluid accumulation in the body. This fluid buildup can affect the respiratory control centers in the brainstem, leading to central sleep apnea. Proper management of congestive heart failure and medications prescribed by a healthcare professional can help alleviate sleep apnea symptoms.
Stroke
A stroke occurs when blood supply to the brain is interrupted, resulting in brain cell damage. Depending on the location and severity of the stroke, it can affect the brainstem and disrupt the breathing process during sleep, causing central sleep apnea. Rehabilitation programs and medical interventions are essential in treating sleep apnea caused by stroke.
Medication Side Effects
Certain medications, particularly opioids and narcotic pain relievers, can depress the central nervous system, including the respiratory centers in the brain. This depression can lead to central sleep apnea episodes. It is important to discuss with healthcare providers any concerns about medication side effects that may contribute to sleep apnea.
This image is property of www.mayoclinic.org.
Complex Sleep Apnea Syndrome
Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when an individual with obstructive sleep apnea develops central sleep apnea after using continuous positive airway pressure (CPAP) therapy to manage their symptoms. The exact cause of this transition is not fully understood, but it may be related to the interaction between the upper airway and brainstem control of breathing. Treating complex sleep apnea syndrome may involve a combination of therapies targeting both obstructive and central components.
Anatomical Factors
Narrowed Airway
Some individuals naturally have a narrower airway, making them more susceptible to sleep apnea. The narrowing of the airway can occur in various parts, such as the nasal passages, throat, or vocal cords. Addressing the root cause of the narrowed airway, such as anatomical abnormalities or inflammation, can help alleviate sleep apnea symptoms.
Large Tongue
A large tongue can contribute to the obstruction of the upper airway during sleep. When the tongue relaxes and falls back, it can block the airflow and lead to apnea episodes. Oral appliances or surgical procedures can be considered to address the anatomical factor of a large tongue and help improve sleep apnea symptoms.
Small Jaw
A small jaw can result in a reduced space for the tongue and other tissues in the mouth, potentially causing airway obstruction during sleep. Orthodontic treatments or oral appliances may be recommended to help reposition the jaw and increase the airway space, leading to improved sleep quality for individuals with sleep apnea.
Misaligned Jaw
A misaligned jaw, also known as temporomandibular joint (TMJ) disorder, can impact the position of the tongue and other structures within the mouth, potentially leading to sleep apnea. TMJ treatments, such as splints or jaw exercises, can help alleviate symptoms and improve the function of the jaw, contributing to better sleep and reduced sleep apnea occurrences.
This image is property of www.verywellhealth.com.
Neuromuscular Disorders
Muscular Dystrophy
Muscular dystrophy is a group of genetic disorders characterized by the progressive weakening and wasting of muscles. As the muscles involved in breathing weaken, individuals with muscular dystrophy may develop sleep apnea. Collaborating with healthcare providers and implementing respiratory support systems, such as non-invasive ventilation, can help manage sleep apnea symptoms in those with muscular dystrophy.
Amyotrophic Lateral Sclerosis (ALS)
ALS, also known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that affects nerve cells responsible for muscle control. As ALS progresses, the muscles involved in breathing weaken, leading to central sleep apnea. Working closely with healthcare professionals to develop a comprehensive treatment plan, which may include assisted ventilation, is crucial in managing sleep apnea symptoms in individuals with ALS.
Hormonal and Metabolic Imbalances
Hypothyroidism
Hypothyroidism, an underactive thyroid gland, can impact metabolism and hormone production in the body. The condition can contribute to weight gain and increased fat deposition in the neck and throat area, leading to obstructive sleep apnea. Treating hypothyroidism with medication and maintaining optimal thyroid function can help manage sleep apnea symptoms.
Acromegaly
Acromegaly is a hormonal disorder characterized by excessive production of growth hormone in adults. The condition can lead to changes in facial structure, including enlarged tongue, tonsils, and adenoids, potentially causing obstructive sleep apnea. Collaborating with endocrinologists and sleep specialists to manage acromegaly and its associated symptoms is essential in addressing sleep apnea in individuals with this condition.
This image is property of www.sleepcareonline.com.
Smoking and Alcohol
Impact on Upper Airway
Smoking and excessive alcohol consumption can directly impact the upper airway, increasing the risk of sleep apnea. Smoking causes inflammation and irritation of the airway tissues, while alcohol relaxes the muscles in the throat and tongue, further contributing to airway collapse during sleep. Quitting smoking and limiting alcohol intake can play a significant role in reducing sleep apnea symptoms and improving overall respiratory health.
Medical Conditions
High Blood Pressure
Sleep apnea and high blood pressure often coexist. The repeated interruptions in breathing during sleep can cause blood oxygen levels to drop, placing strain on the cardiovascular system and leading to hypertension. Treating sleep apnea through lifestyle modifications, such as weight loss and continuous positive airway pressure (CPAP) therapy, can help manage high blood pressure and reduce cardiovascular risks.
Diabetes
There is a strong link between sleep apnea and diabetes. People with diabetes are more likely to develop sleep apnea, and untreated sleep apnea can negatively affect blood sugar control. The combination of both conditions can increase the risk of cardiovascular complications. Treating sleep apnea and effectively managing diabetes with lifestyle changes and medication can significantly improve overall health outcomes.
Congestive Heart Failure
Congestive heart failure can contribute to the development of sleep apnea, as mentioned earlier in the central sleep apnea section. The fluid buildup associated with heart failure can affect the brainstem’s respiratory control centers, leading to interruptions in breathing during sleep. Proper management of congestive heart failure and coordination of care between healthcare providers is essential in addressing sleep apnea in individuals with this condition.
Stroke
Individuals who have had a stroke are at an increased risk of developing sleep apnea. Depending on the location and severity of the stroke, the brainstem’s respiratory control centers can be affected, leading to interrupted breathing during sleep. Rehabilitation programs and close monitoring of sleep apnea symptoms are vital in stroke recovery and overall management.
Heart Disorders
Various heart disorders, such as arrhythmias or structural abnormalities, can contribute to sleep apnea. These conditions can impact the electrical signals and blood flow within the heart, leading to disturbances in breathing during sleep. Collaborating with cardiologists and sleep specialists can help assess and manage both cardiac conditions and sleep apnea, improving overall cardiovascular health.
This image is property of www.nhlbi.nih.gov.
Family History and Genetics
Inherited Traits
Sleep apnea can run in families, suggesting a genetic predisposition to the condition. If individuals have family members who have been diagnosed with sleep apnea, they may have an increased risk of developing the disorder themselves. While genetics alone may not cause sleep apnea, it is important to be aware of the potential familial connection and take proactive steps to manage risk factors.
Genetic Disorders
Certain genetic disorders, such as Down syndrome or Pierre Robin sequence, are known to be associated with sleep apnea. These disorders can lead to anatomical abnormalities in the airway or interfere with respiratory control mechanisms, increasing the likelihood of sleep apnea. Close monitoring and intervention by healthcare professionals are crucial in addressing sleep apnea in individuals with genetic disorders.
Age and Gender
Advanced Age
Sleep apnea becomes more prevalent as individuals age. The aging process can lead to changes in muscle tone and structure, including the muscles involved in breathing. The relaxation of these muscles during sleep can result in airway blockages and sleep apnea. Regular sleep assessments and appropriate treatments are essential in managing sleep apnea as individuals age.
Males vs Females
Sleep apnea is more commonly diagnosed in males than females, although it can affect individuals of all genders. The differences in anatomy and hormone levels between males and females may contribute to this gender disparity. However, it is important to note that women can still develop sleep apnea, especially during hormonal changes such as pregnancy or menopause. Awareness of sleep apnea symptoms in both males and females is crucial for early detection and effective management.
In conclusion, sleep apnea can be caused by a variety of factors. Obstructive sleep apnea is often linked to excess weight, upper airway obstructions, anatomical factors, neuromuscular disorders, hormonal and metabolic imbalances, smoking, alcohol use, and certain medical conditions. Central sleep apnea is primarily caused by brainstem problems, congestive heart failure, stroke, or medication side effects. Complex sleep apnea syndrome involves a combination of obstructive and central factors. Understanding the causes of sleep apnea is essential in developing tailored treatment plans to alleviate symptoms and improve overall quality of life. If you suspect you or a loved one may have sleep apnea, it is important to consult with a healthcare professional for proper evaluation and diagnosis.
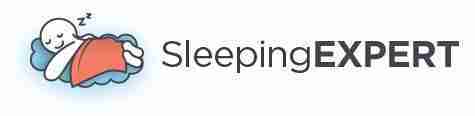
This image is property of my.clevelandclinic.org.